by NATASHA GILBERT
Increasingly sensitive tests have raised the risk overdiagnosis. Understanding a person’s chance of disease could reduce the harmful side effects of screening.
Impotence and incontinence are common side effects of treatment for prostate cancer. For men with aggressive forms of the disease, these treatment consequences will outweigh the alternative — prostate cancer is one of the biggest cancer killers in men. But a large proportion of people diagnosed with prostate cancer are treated for slow-growing tumours that would have been unlikely to cause harm if left alone — the potential side effects of treatment overshadow the gains.
These people are treated because their cancers are flagged by screening programmes. Overdiagnosis and overtreatment are also common outcomes of breast-cancer screening, leading researchers to question whether screening for these cancers is doing more harm than good.
“Used wisely, screening for breast and prostate cancer can significantly reduce an individual’s risk of dying from those cancers. However, the potential benefits may not necessarily outweigh the expected harms and costs of screening on a population level,” says Sigrid Carlsson, an epidemiologist at the Memorial Sloan Kettering Cancer Center in New York.
Screening for cancer is designed to catch disease early, when physicians have the best chance of treating it. But differences in opinion over the benefits of breast- and prostate-cancer screening have led to confusing and contradictory recommendations about which people to screen, when and how often. Screening for other types of cancer such as colorectal and cervical cancer is less controversial because they tend to be slower growing, more homogeneous and more readily detected and removed with fewer serious side effects, say researchers.
Scientists are trying to resolve the issues over breast- and prostate-cancer screening by developing more-accurate screening tools. One persistent theme is the push for an individualized approach — each person’s risk is assessed in a way that allows them to make an informed decision.
Harmful effects
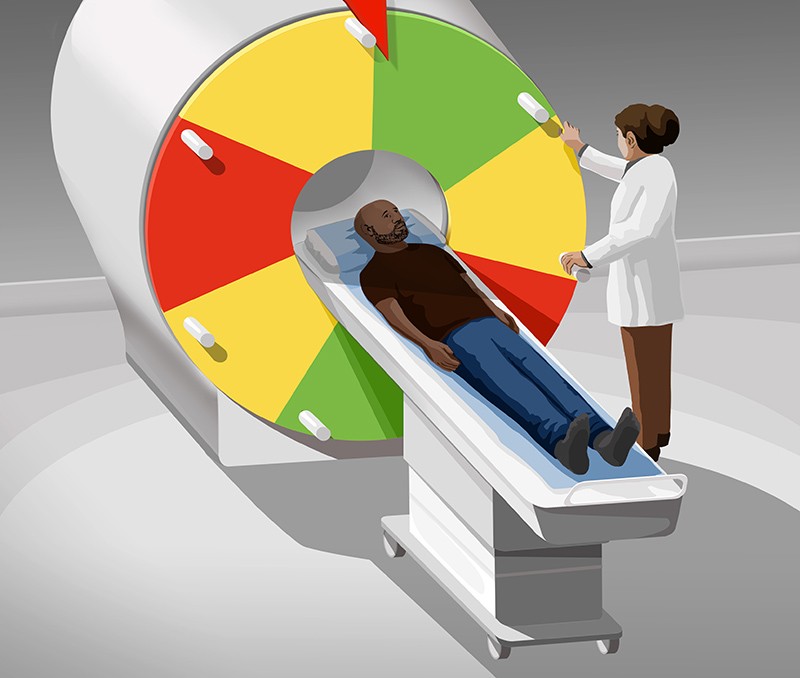
Prostate and breast cancer account for around one-quarter of all new cancer diagnoses in the United States, according to data from the American Cancer Society. The common occurrence of these cancers is partly due to widespread screening practices that began in the 1980s and 1990s. Breast-cancer screening typically uses a mammogram — a low-energy X-ray of the breast to look for masses that can’t be seen or felt through physical examination. Prostate-cancer screening involves testing the blood for elevated levels of prostate-specific antigen (PSA), a protein produced by the prostate gland.
Nature for more