by LYNNE PEEPLES
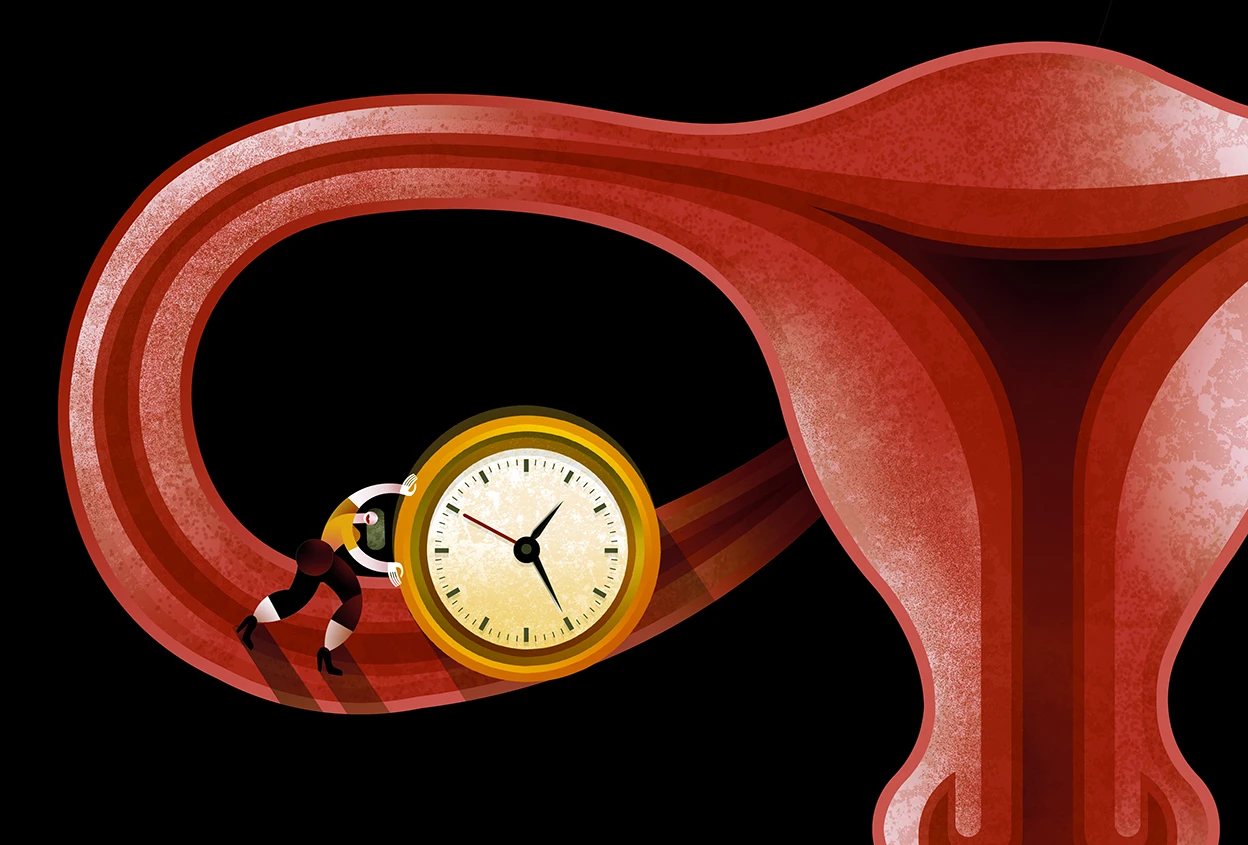
Researchers are exploring how to prolong ovarian life and revisiting hormone replacement therapy — a once routine treatment that has fallen out of favour.
In late 2022, Naomi Busch, a lone physician in her book group, began fielding question after question about menopause. Members of the group had started to experience the hallmark symptoms — hot flushes, poor sleep and mood swings — and wondered what they could do about them. “They all looked at me,” says Busch, “and I was like, ‘I don’t know anything about menopause.’” She searched for knowledgeable physicians in and around Seattle, where she lives, but the few specialists were booked out for several months. Meanwhile, the women in the book group were not getting the answers that they needed from their gynaecologists or primary-care physicians. “I’m not going down quietly,” Busch remembers one woman vowing.
Busch, who trained in and practised primary-care medicine, wasn’t surprised by the lack of information. “It’s not something we learn about in medical school,” she says. So Busch decided to find out everything she could about menopause. Ultimately, she passed a competency exam to become a certified practitioner through The Menopause Society, a non-profit organization based in Pepper Pike, Ohio, that provides tools and resources to health-care professionals. She’s not alone in her interest. More than 1,300 providers became certified in 2024; and more than five times as many people applied for the exam in 2024 as in 2022. The International Menopause Society, a UK-based charity, also offers a free online training programme for health-care professionals. More than 2,600 people completed the course in 2024, up from under 2,000 in 2023.
Many health-care professionals — along with society in general — regularly tell women, and transgender, non-binary and intersex people who go through menopause, to accept the misery of the transition, and the health troubles that can follow. Menopause comes with increased risks of health conditions such as cardiovascular disease, diabetes, osteoporosis and memory loss.
Yet, few medical options are typically presented to people going through menopause. Sometimes, oral contraceptives are prescribed to ease symptoms and prevent unwanted pregnancies, which are still possible during the transition. But common doses and formulations can include risks, such as developing blood clots, and don’t always provide sufficient treatment, says Busch. Non-hormonal drugs, such as fezolinetant and elinzanetant, treat hot flushes — but they also have side effects. Other options include antidepressants, cognitive behavioural therapy, acupuncture and lifestyle changes, which usually go only so far in alleviating symptoms. Hormone replacement therapy, which was a routine treatment until 2002, is widely passed over, owing to a misinterpreted study1 that prompted fear of its use.
Nature for more
